Chest Pain Acute Coronary Syndrome
Section 4 - CARDIAC
4.01 CHEST PAIN/ACUTE CORONARY SYNDROME
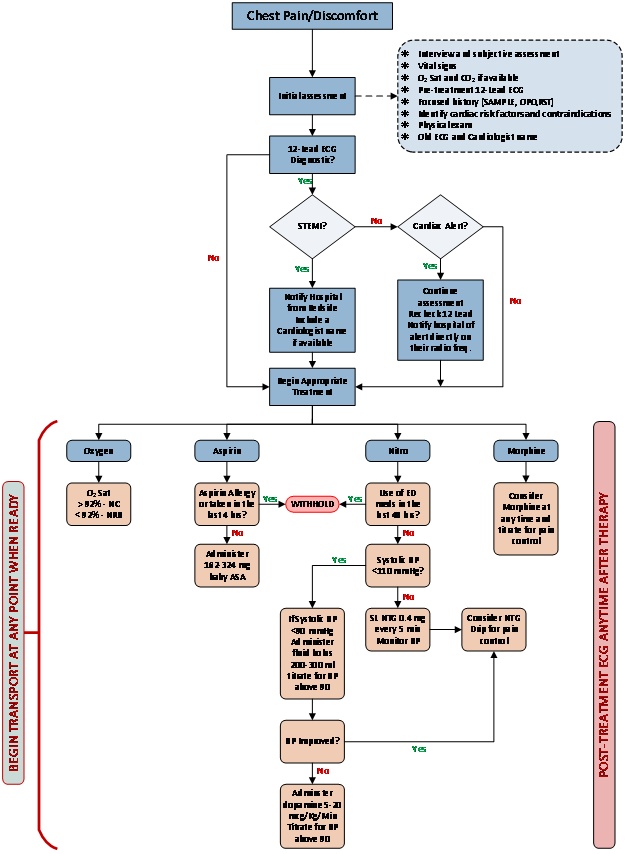
Perform initial assessment:
- Interview and subjective assessment
- Vital signs
- Oxygen saturation and sideline/sidestream capnography if available
- Pre-treatment 12-Lead ECG
- Focused history (SAMPLE, OPQRST)
- Identify cardiac risk factors and contraindications for Fibrynolytics
- Physical exam
- Inquire if the patient has an old ECG and Cardiologist name
Indications for 12-Lead ECG include but are not limited to:
- Chest pain/discomfort
- Palpitations/dysrhythmias
- Shortness of breath
- Syncope/dizziness
- Feelings of “impending doom”
- Sweating nausea or vomiting
- Beware of atypical presentations (absence of chest pain) in women, diabetics & geriatric patients.
If Symptoms, Chief Complaint and 12-Lead diagnostic pre-treatment ECG evaluation suggests angina/ myocardial infarction, consider one of the following notifications:
“STEMI ALERT” (ST ELEVATION MI) – If the 12-Lead diagnostic ECG evaluation indicates ONE of the following findings:
- ST elevation > 1.0 mm present in two (2) or more inferior leads
- ST elevation > 2.0 mm in two (2) or more precordial leads
When transporting a STEMI to the ED of any hospital, have your EKG strip initialed by the attending physician verifying the STEMI or not. Please ask the physician to initial, date and to indicate “Yes” or “No” to certify the correct diagnosis of STEMI or not. If you are unable to have the physician initial at the time of your transport you may have him do it the next time you are at the ED.
“CARDIAC ALERT” – If 12-Lead diagnostic ECG evaluation indicates ONE of the following findings:
- New bifascicular block (RBBB) with QRS axis deviation of > -50
- Signs of ischemia such as: new inverted T-Waves or ST depression in two (2) or more contiguous leads
- Normal ECG with signs and symptoms of Myocardial infarction
- New Left Bundle Branch Block (LBBB)
- Hyper-acute T waves present in two or more contiguous leads
- Onset of any new arrhythmia
TREATMENT:
- Consider MORPHINE, OXYGEN, NITROGLYCERIN TABLETS OR NITROGLYCERIN SPRAY AND ASPIRIN (MONA)
- Administer OXYGEN, nasal cannula if saO2 > 92%; non-rebreather if saO2 < 92%.
- If systolic BP > 110 mm Hg: NITROGLYCERIN SPRAY or NITROGLYCERIN TABLETS 0.4 mg SL (Do not withhold if unable to establish IV). Repeat at 5 minute intervals until either systolic BP < 110 mm Hg or NITROGLYCERIN drip established. (Team member should be assigned as “nitro-time keeper”)
| Black Box Warning |
|---|
| The administration of sublingual nitroglycerin is CONTRAINDICATED if the patient taking daily doses of or has a recent history (36-48 hrs) of using any type of erectile dysfunction medications from the phosphodiesterase type 5 (PDE-5) class such as Sildenafil Citrate (Viagra), Vardenafil (Levitra) or Tadalafil (Cialis).
|
- If systolic BP > 110 mm Hg, NITROGLYCERIN DRIP, START at 5-15 mcg/minute via Infusion Regulator (Dial-a-Flow device) or Buretrol device. Titrate and increase NITROGLYCERIN DRIP at 5 mcg/minute increments every 3-5 minutes until relief of discomfort. Establish second IV of NaCl, however keep in mind the patient may be a candidate for Thrombolytics. Monitor and document BP every 5 minutes. If pain is relieved, leave drip at setting when relief occurred.
If pain is not relieved and/ or more severe- follow initial nitro drip infusion with MORPHINE SULFATE administration Refer to ANALGESIA/SEDATION PARAMETERS (2.04)
- BABY ASA 162 – 324 mg, chewed.
- Evaluate and treat the patient’s pain level. Pain level equal to or greater than 4 must be treated with a goal in the reduction of pain severity to a level of 2 or less.
- Obtain additional 12-lead ECG, post-treatment of patient.
- Perform blood draw of all tubes. The crew shall hold onto the tubes at the hospital until a staff member is ready to label the blood tubes. Document that blood was drawn.
- If patient has vomiting or severe nausea, obtain detailed history and administer an Antiemetic medication as appropriate.
- If systolic BP < 90 mm Hg, consider fluid boluses in increments of 200 - 300 ml, to titrate systolic BP > 90 mm Hg. Monitor for signs of fluid overload.
- If condition worsens despite fluid therapy, administer DOPAMINE 5 - 20 mcg/kg/minute titrated to systolic BP > 90 mm Hg.
Remove transdermal patches to avoid excessive dosing. (Transdermal patches may also cause electrical arcing during defib or cardioversion).
Vasovagal reaction may occur. It is usually transient and responds to elevating the patient’s legs. ATROPINE may be used but is rarely necessary.
TRANSPORT DESTINATION
- Patients with identified STEMI/Cardiac alerts must be transported to a STEMI receiving facility.
- Current STEMI receiving facilities:
- AdventHealth Altamonte
- Orlando Health Lake Mary
- HCA Florida Lake Monroe Hospital
- AdventHealth Orlando
- AdventHealth Apopka
- Orlando Regional Medical Center