Ventricular Fibrillation Pulseless Ventricular Tachycardia: Difference between revisions
No edit summary |
|||
| Line 48: | Line 48: | ||
** VF/VT Present – deliver a DEFIBRILLATION 300-360j biphasic | ** VF/VT Present – deliver a DEFIBRILLATION 300-360j biphasic | ||
** Subsequent shocks should be at the higher dose selected | ** Subsequent shocks should be at the higher dose selected | ||
''If after 3 attempts at defibrillation and patient is still presenting VF, each subsequent shock should be delivered at '''''720j biphasic'''''(using [https://www.youtube.com/watch?v=Ov-BBUhKdJU double sequential defibrillation]) | |||
* Administer antidysrhythmic medication: | * Administer antidysrhythmic medication: | ||
** [[Antiarrhythmics|AMIODARONE]] 300 mg IVP, IO. | ** [[Antiarrhythmics|AMIODARONE]] 300 mg IVP, IO. | ||
Revision as of 17:01, 28 December 2016
Section 4 - CARDIAC
4.08 CARDIAC ARREST - VENTRICULAR FIBRILLATION /PULSELESS VENTRICULAR TACHYCARDIA
Ventricular Fibrillation (VF) and Pulseless V-Tach (VT) focuses in the correction of the dysrhythmia into a pulse producing rhythm. Consider all possible reversible causes for cardiac arrest utilizing a national recommended mnemonic of “H’s and T’s”:
| H’s | T’s |
|---|---|
| Hypovolemia | Tension Pneumothorax |
| Hypoxia | Tamponade, cardiac |
| Hydrogen Ion (acidosis) | Toxins or Tablets (overdose) |
| Hypo/hyperkalemia | Thrombosis, pulmonary |
| Hypothermia | Thrombosis, cardiac |
In addition, also consider the following:
| Hypoglycemia | Trauma |
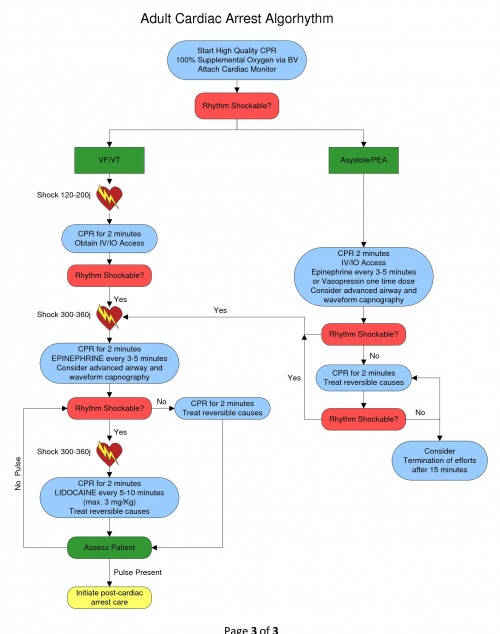
When the Patient found in cardiac arrest:
- Initiate BLS algorhythm with 5 cycles of high quality CPR (push hard/push fast)
- Minimum of 100 compressions per minute, minimize interruptions
- Compression rate of 30:2 for approximately 2 minutes
- Depth of compression of at least 2 inches
- Initiate the use of a mechanical compression device if available
- Assist ventilations with OXYGEN @ 100% via BVM - DO NOT HYPERVENTILATE
- Attach cardiac monitor – Evaluate the cardiac rhythm
- VF/VT Present – deliver a DEFIBRILLATION 120-200j biphasic
- Continue high quality CPR/Ventilations for 2 minutes
- Establish intravenous access via IV or IO
- Consider advanced airway procedure using supraglottic airway (king tube) or endotracheal intubation
- Do not interrupt compressions to place an advanced airway
- Confirm tube placement with capnography (a range 5-20 mmHg is indicative of low cardiac output)
- Administer EPINEPHRINE 1:10,000 1 mg IV / IO – repeat every 3-5 minutes of arrest
- OR
- Administer VASOPRESSIN 40 units IV / IO – replaces the first or second dose of epinephrine
- Vasopressin is a one-time dose
- Do not stop CPR to administer medications
- Reassess for circulation every two minutes
- VF/VT Present – deliver a DEFIBRILLATION 300-360j biphasic
- Subsequent shocks should be at the higher dose selected
If after 3 attempts at defibrillation and patient is still presenting VF, each subsequent shock should be delivered at 720j biphasic(using double sequential defibrillation)
- Administer antidysrhythmic medication:
- AMIODARONE 300 mg IVP, IO.
- May repeat second dose AMIODARONE (if needed) 150 mg IV, IO in 3-5 minutes.
- Maximum dose 450 mg.
- OR
- Administer LIDOCAINE 1 to 1.5 mg/kg IVP, IO. May repeat every 5-10 minutes to a maximum of 3 mg/Kg.
- In patients over age 70 or in those with known hepatic disease, administer LIDOCAINE gradually up to a full initial loading dose or until a maximum of 1.5 mg/kg administered.
- If VF/VT converts to a pulse-producing non-heart block supraventricular rhythm, administer a LIDOCAINE DRIP 1-4 mg/min.
- In patients over age 70 or in those with known hepatic disease, administer LIDOCAINE DRIP at the lower 1-2 mg/min. MONITOR FOR SIGNS OF TOXICITY including seizure activity.
- Administer MAGNESIUM SULFATE 2 gm IVP only if suspected Polymorphic VT (Torsades de pointes) or hypomagnesemic state (chronic alcohol, diuretic use)
- Administer SODIUM BICARBONATE 1 mEq/kg IVP if suspected, HYPERKALEMIA (e.g. dialysis patient), or Tricyclic antidepressant OD
If patient combative post resuscitation, refer to ANALGESIA / SEDATION PARAMETER (2.04)
Deliver all Defibrillations at 360 Joules in any patient who has had an Automatic Implanted Cardioverter Defibrillator (AICD) shock. (Use Anterior/Posterior position if possible for Defibrillator Pads - Do not place pads over device).
- Consider sedation in patient experiencing cardioversion or defibrillation by their own AICD.
- Leave copy of ECG at ER on any patient with implanted device.